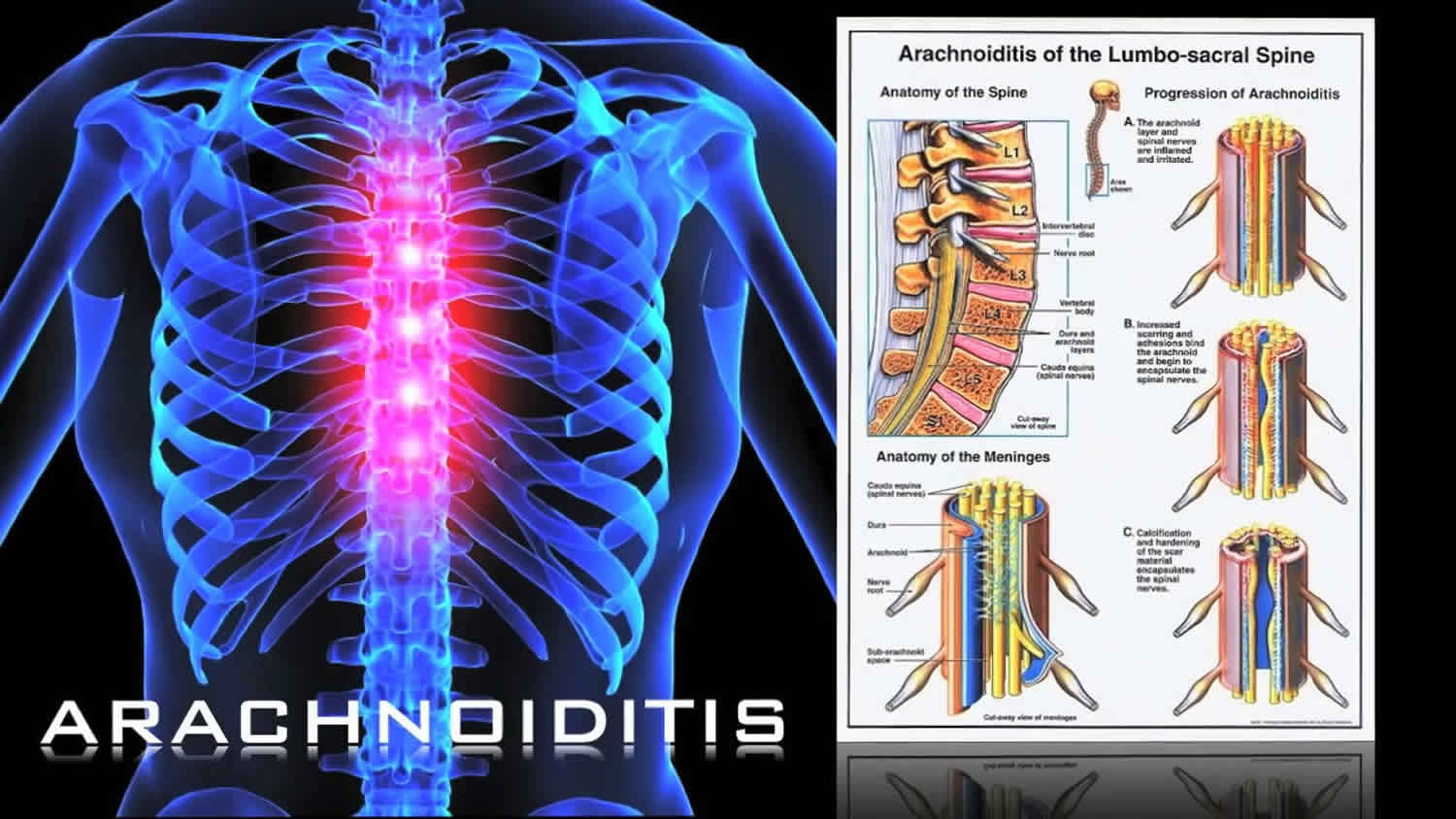
Adhesive arachnoiditis is a neurological disorder caused by the scarring and inflammation of the arachnoid membrane, a layer of tissue that covers the spinal cord and brain. It is a progressive disorder that can cause pain and neurological dysfunction. Symptoms may include numbness, tingling, burning, and muscle weakness. In some cases, the disorder can cause paralysis and bladder or bowel problems. Adhesive arachnoiditis is usually caused by an infection or an injury to the spinal cord or brain, often due to a procedure like a lumbar puncture.
It can also be caused by an allergy to certain medications. Treatment for adhesive arachnoiditis is usually focused on relieving the symptoms and can include medications, physical therapy, and lifestyle changes. Surgery is usually not recommended, as it can cause more scarring and pain. Adhesive arachnoiditis is a serious neurological disorder and can have a significant impact on a person’s life. It is important to seek medical attention if any of the symptoms described above are experienced.
How is adhesive arachnoiditis diagnosed

The diagnosis of adhesive arachnoiditis is usually done through an MRI or CT scan. These imaging tests help to identify any scarring or damage to the arachnoid membrane. The doctor may also do a physical examination, nerve conduction studies, and lumbar puncture (LP), which is a spinal tap that helps to check the pressure in the spinal column. In some cases, your doctor may also order a myelogram, which is an X-ray imaging test that can help to identify any defects in the spinal cord. Additionally, your doctor may also perform an electromyography (EMG) which is a test that measures the electrical activity of the muscles.
Adhesive arachnoiditis is a difficult disorder to diagnose because the symptoms can be similar to other neurological diseases. Because of this, it is important to get a comprehensive medical evaluation to determine the cause of your symptoms. Finally, the doctor may also recommend lifestyle changes to help manage the symptoms and improve quality of life. These lifestyle changes may include physical therapy, medications, and stress management. Making lifestyle changes can help reduce the severity of the symptoms and improve your overall health and wellbeing.
How do you know if you have adhesive arachnoiditis?
The most common symptom of adhesive arachnoiditis is persistent pain. Other symptoms can include headaches, sensitivity to light and sound, nausea, fatigue, and difficulty with concentration and coordination. If you experience any of these symptoms, it is important to see a doctor as soon as possible. A physical exam and imaging tests can help determine if you have adhesive arachnoiditis. Your doctor may also recommend other tests such as a lumbar puncture, which can detect inflammation of the arachnoid mater.
In some cases, a biopsy of the affected area may be needed to diagnose adhesive arachnoiditis. Treatment for adhesive arachnoiditis can include medications to reduce inflammation, physical therapy to reduce pain and improve mobility, and surgery to remove scar tissue or other abnormal tissue in the arachnoid mater. Consulting with a specialist can help determine the best treatment plan for you.
Is arachnoiditis seen on MRI?
The diagnosis of Adhesive Arachnoiditis requires a physical examination and diagnostic tests, such as an MRI. MRI scans can show evidence of inflammation and adhesive changes in the arachnoid membrane. Imaging can also help to identify the cause of the arachnoiditis. In cases of Adhesive Arachnoiditis, the MRI may show thickening of the arachnoid membrane and changes in surrounding structures, including the spinal cord, nerve roots, and veins. The MRI may also reveal the presence of cysts and other abnormalities.
The MRI scan may also reveal compression of the nerve roots and spinal cord, which can cause pain and other neurological symptoms. MRI scans may also reveal fluid collections in the spinal canal, which can further compress and irritate the nerve roots. Adhesive Arachnoiditis is a serious condition that can cause severe pain and neurological problems. It is important to get a diagnosis as soon as possible so that appropriate treatment can be started. An MRI may be required to diagnose adhesive arachnoiditis, and it can help to identify the cause and other abnormalities in the arachnoid membrane.
How fast does adhesive arachnoiditis progress?
The exact rate of progression of adhesive arachnoiditis is hard to predict, as it can vary from person to person. Generally, the condition can progress slowly over time, with symptoms becoming more severe. In some cases, it can remain at a stable level, while in others it can progress quickly. The symptoms of adhesive arachnoiditis can include pain in the lower back and legs, numbness, weakness, and tingling in the limbs, bladder and bowel difficulties, and fatigue. As the condition progresses, these symptoms can become more severe and more widespread.
Treatment for adhesive arachnoiditis is primarily aimed at reducing the inflammation and managing the symptoms. In some cases, surgery may be offered to relieve the pressure on the nerves in the spine. Medications can also be used to relieve the pain and inflammation. Overall, adhesive arachnoiditis can progress at different speeds for different people. It is important to speak to a doctor if you are experiencing any of the symptoms associated with the condition, so that the appropriate treatment can be recommended.
What does adhesive arachnoiditis look like on MRI?
It causes a plethora of symptoms including chronic pain, difficulty walking, and bladder dysfunction. On MRI scans, adhesive arachnoiditis is often characterized by a thin, dark line around the spinal cord. This dark line is caused by the inflammation of the nerve roots and membranes of the spinal cord and is known as a ‘dural tail’ sign. Other imaging features of adhesive arachnoiditis include bilateral post-laminar enhancement and a diffusely increased signal intensity on T2-weighted images. The enhancement of the post-laminar structures is caused by the accumulation of proteinaceous materials in the subarachnoid space.
In advanced cases of adhesive arachnoiditis, the signs can become more pronounced. This includes the appearance of multiple dural tails, increased post-laminar enhancement, and an even greater increase in signal intensity on T2-weighted images. Adhesive arachnoiditis is an often debilitating condition. MRI scans can be used to detect and monitor the condition, and in some cases, to offer potential treatments.
What kind of doctor treats arachnoiditis?
The most common type of doctor that treats arachnoiditis is a neurologist. Neurologists specialize in diagnosing and treating diseases that affect the nervous system. They often work closely with other specialists, such as physical therapists and occupational therapists, to develop customized treatment plans for their patients. To diagnose adhesive arachnoiditis, a neurologist may conduct a physical exam, order imaging tests such as a CT or MRI scan, and evaluate the patient’s reflexes and sensory function. They may also perform a spinal tap to assess the fluid surrounding the spine.
Treatment for arachnoiditis usually involves medications to reduce inflammation and relieve pain, physical therapy to improve mobility and strength, and lifestyle changes to accommodate the condition. In some cases, surgery may be necessary to remove scar tissue or repair herniated discs. If left untreated, adhesive arachnoiditis can cause permanent nerve damage. Therefore, it is important to seek prompt medical attention if you experience any of the signs or symptoms of this condition. A neurologist can help diagnose your condition and provide personalized treatment to help reduce your pain and improve your quality of life.
Is there a blood test for arachnoiditis?
Symptoms of adhesive arachnoiditis may include pain, tingling, and muscle weakness. People can also experience problems with their bladder, bowel, and/or sexual function. Unfortunately, there is no definitive test for adhesive arachnoiditis, although it can be diagnosed through an MRI or CT scan. Additionally, there is no blood test for accurately diagnosing the condition. Treatment for adhesive arachnoiditis may include medications to reduce inflammation, physical therapy, and lifestyle modifications.
Surgery is usually not recommended, as it can make the condition worse. Adhesive arachnoiditis is a serious condition, and it is important to receive proper medical advice if you think you may be experiencing symptoms. Early diagnosis and treatment can help to reduce symptoms and improve quality of life.
What kind of doctor do you see for arachnoiditis?
The exact cause of adhesive arachnoiditis is not known, but it is thought to be related to infection, inflammation, and trauma to the spinal cord. It can also be caused by the use of certain medications injected into the spinal cord, such as steroids and anesthetics. If you have adhesive arachnoiditis, you should see a neurologist or a spine specialist. They can determine the extent of your condition and recommend the best treatment option for your particular case. Treatment options may include physical therapy, medications, and in some cases, surgery.
Your doctor may also recommend that you see a physical therapist for exercises to help with your recovery. A physical therapist can help you learn stretches and exercises that can improve your strength, flexibility, and range of motion. If you have adhesive arachnoiditis, it is important to follow your doctor’s instructions carefully, and seek out help from all the appropriate professionals in order to manage the condition and reduce your pain and disability.
What does adhesive arachnoiditis feel like?
This inflammation results in scar tissue that binds the arachnoid membrane to the underlying dura mater, which can cause chronic pain and other symptoms. The pain of adhesive arachnoiditis is often described as a burning, stabbing, or tingling sensation that can be felt throughout the body. It may be localized to certain regions, such as the lower back, or may be diffuse and widespread. A person with adhesive arachnoiditis may also experience numbness, weakness, loss of sensation, and other neurological deficits. Adhesive arachnoiditis can be an extremely debilitating condition and the symptoms may vary wildly from person to person.
In some cases, the pain may be mild and intermittent, while in others it may be severe and constant. The effects of the condition can be so severe that even a slight change in position can cause excruciating pain. The effects of adhesive arachnoiditis can be both physical and psychological. A person with the condition can struggle with intense pain, fatigue, anxiety, depression, and insomnia. They may also experience cognitive deficits, memory problems, and difficulty with coordination. Adhesive arachnoiditis can be a difficult condition to live with, but it is important to remember that there are effective treatment options. A combination of physical therapy, medications, and lifestyle changes can help improve the symptoms of adhesive arachnoiditis and improve quality of life.
Can an MRI diagnose adhesive arachnoiditis?
What is adhesive arachnoiditis? Adhesive arachnoiditis is a rare condition, in which the arachnoid membrane, a layer of tissue that covers the brain and spinal cord, becomes irritated and inflamed. This inflammation is usually caused by a prior medical procedure, such as a lumbar puncture, or due to exposure to certain chemicals. The inflammation can cause a variety of symptoms, including severe headaches, pain, sensory changes, and difficulty with bladder and bowel control. In some cases, the condition may even lead to paralysis. Can an MRI diagnose adhesive arachnoiditis? Yes, an MRI is sometimes used to diagnose adhesive arachnoiditis.
An MRI is a non-invasive imaging technique which produces detailed images of the brain and spinal cord. An MRI scan can reveal the presence of inflammation and scarring in the arachnoid membrane, allowing for a diagnosis to be made. Additional tests, such as a lumbar puncture or a spinal tap, may be necessary to confirm the diagnosis. These tests will help to identify any underlying causes of the inflammation, such as a bacterial or viral infection. Adhesive arachnoiditis is a serious condition, and treatment should not be delayed. If you believe you may be suffering from adhesive arachnoiditis, it is important to see a doctor as soon as possible. An MRI scan can help to diagnose the condition, and appropriate treatment can be started to reduce symptoms and improve quality of life.
What are the symptoms of arachnoiditis?
This condition can lead to a number of painful, disabling symptoms. The most common symptom of arachnoiditis is back pain, which is often chronic and difficult to manage. It can range from a mild ache to a stabbing, burning sensation. Other symptoms may include muscle weakness, numbness or tingling in the extremities, and difficulty walking or standing. Some patients may also experience bladder or bowel problems, such as incontinence or constipation.
In addition to physical symptoms, arachnoiditis can lead to severe emotional distress and depression. Many patients with this condition suffer from a diminished quality of life and can no longer take part in activities they used to enjoy. Various imaging techniques and medical tests can help diagnose arachnoiditis, including MRI scans, CT scans, and EMG testing. Treatment typically involves managing the symptoms, as there is currently no definitive cure for the condition. Medications, physical therapy, and lifestyle changes may help reduce pain and discomfort. Some patients also benefit from alternative therapies such as yoga and acupuncture. Adhesive arachnoiditis is a serious condition that can significantly affect a person’s quality of life. It is important to be aware of the symptoms and seek medical advice if any of them occur.
What are the treatment options for adhesive arachnoiditis?
The main treatment options for adhesive arachnoiditis are pain management, physiotherapy, and surgery. These three treatments all focus on relieving and managing pain, as well as improving overall mobility. Pain management may involve medications such as anti-inflammatory drugs, muscle relaxants and opiates. Physiotherapy can also be used to improve strength and posture, as well as improve range of motion. Surgery may be an option if there is an underlying cause of the arachnoiditis, such as a herniated disc or spinal stenosis.
Other less invasive treatments may also be used to treat adhesive arachnoiditis such as acupuncture, massage, biofeedback and electrical stimulation. These treatments are aimed at reducing pain without the use of drugs. Cold and heat therapy may also be used to reduce inflammation and help relieve pain. In extreme cases, a spinal cord stimulator may be implanted to help reduce pain signals. This device sends electrical impulses to the brain, which can block the transmission of pain signals. In addition to treating the symptoms, it is important to focus on lifestyle factors such as diet, exercise, and stress management. Eating a healthy diet and getting regular exercise can help to reduce inflammation and improve overall health. Stress management techniques such as yoga, meditation and deep breathing can also help to reduce pain and improve overall well-being.
What is the history of adhesive arachnoiditis?
The history of this condition dates back to the 1800s, when symptoms of adhesive arachnoiditis were first reported in medical journals. Initially, there was little known about the condition and the cause was unknown. In the 1930s, researchers began to understand that adhesive arachnoiditis was caused by exposure to anesthetic agents, particularly when injected directly into the spinal canal. By the 1940s, adhesive arachnoiditis had become a recognized condition and the medical community began to look for treatments. During the following decades, research into the condition continued and new treatments were developed.
In the 1990s, the introduction of newer anesthetic agents with fewer side effects reduced the occurrence of adhesive arachnoiditis, although cases continued to be reported. Today, it is widely accepted that adhesive arachnoiditis has a variety of possible causes including direct injection of anesthetic agents, trauma, infection, and the presence of certain medical implants. Treatments vary depending on the severity of the condition, but physical therapy, pain management, and surgery are common options.
How do you get adhesive arachnoiditis
Symptoms may include pain, weakness, numbness, and sensory disturbances in the lower parts of the body. There is no one definitive way to get adhesive arachnoiditis. It is caused by a variety of factors, including surgical intervention, trauma, infection, and toxic exposure. It is most commonly caused by a procedure known as a lumbar puncture, in which a needle is inserted into the lower part of the spine to collect a sample of cerebrospinal fluid. Other potential causes of adhesive arachnoiditis include spinal injury due to falls or accidents, infection of the spinal cord or brain, and exposure to certain toxins or medications.
In some cases, the condition may develop without any apparent cause. Diagnosis of adhesive arachnoiditis is made through a combination of physical examination, imaging studies, and laboratory testing. Common diagnostic tests include MRI scans, CT scans, lumbar puncture, and biopsy. Treatment is generally focused on managing pain and other symptoms. This may include medications, physical therapy, and lifestyle changes. In some cases, surgery may be necessary to relieve pressure on the spinal cord. Adhesive arachnoiditis is a serious condition that can lead to long-term disability. It is important to identify the cause of the disorder and take steps to manage it appropriately. Early diagnosis and treatment is the best way to reduce the risk of long-term complications.
How long does it take for arachnoiditis to develop?
This condition is often caused by trauma to the spinal cord, infection, or repeated spinal injections. As the name suggests, adhesive arachnoiditis is the sticking together of the nerves and the nerve roots, causing inflammation, pain, and an increase in intracranial pressure. The exact amount of time it takes for arachnoiditis to develop depends on the severity of the trauma, infection, or injection. Generally, it can take anywhere from several weeks to several months for symptoms to appear after the initial trauma or infection. In some cases, the symptoms may take longer to develop, and it’s possible for arachnoiditis to remain dormant for years before the symptoms become noticeable. Regardless of the amount of time it takes to develop, adhesive arachnoiditis is a serious condition that can lead to severe pain and disability. There is no known cure for this condition, but there are treatments available to help manage symptoms.
How many stages does arachnoiditis have?
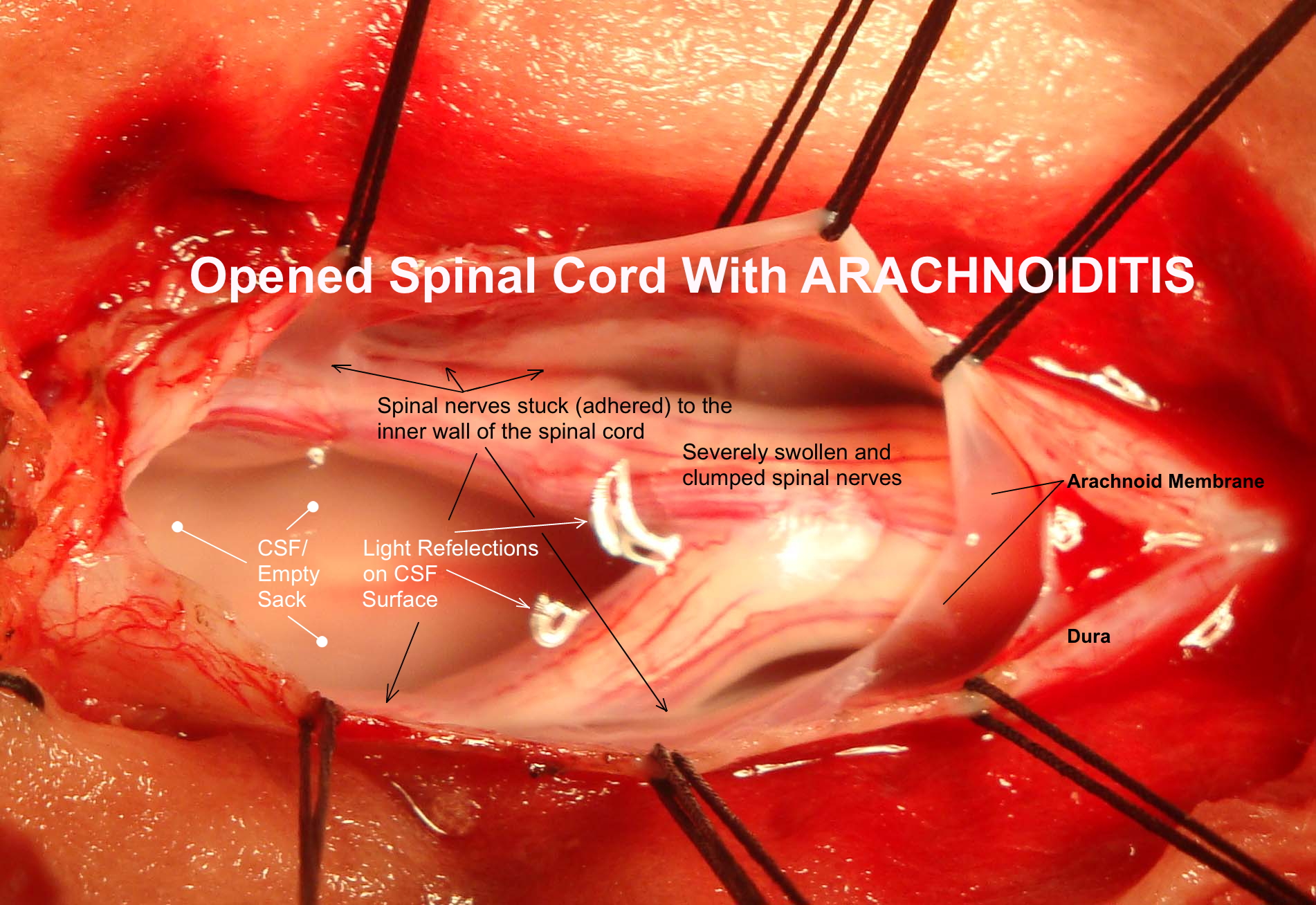
This disorder is divided into three distinct stages, beginning with an initial stage of inflammation which can lead to scarring and adhesion of the arachnoid. In the second stage, the scarring can cause inflammation and pain. In the third and final stage, the scarring has a much greater impact, causing significant nerve irritation and pain. In the early stages of arachnoiditis, the symptoms may be mild, but as the condition progresses, the symptoms become increasingly severe. At the advanced stage of adhesive arachnoiditis, the symptoms can include severe pain and numbness, weakness and paralysis.
In some cases, the symptoms may even lead to permanent disability or paralysis. The three stages of adhesive arachnoiditis are important to note as they can help determine the best treatment option for an individual. It is important to seek medical attention if you suspect you may have adhesive arachnoiditis in order to determine the best course of action for your condition. Early diagnosis and treatment may be able to prevent the progression of the disorder and reduce the severity of the symptoms.
Is adhesive arachnoiditis hereditary?
What is adhesive arachnoiditis? Adhesive arachnoiditis is a painful and debilitating chronic inflammatory disorder of the central nervous system caused by the presence of fibrous adhesions formed between the arachnoid membrane and the underlying structures of the spinal cord. It can cause a variety of neurological symptoms including sensory, motor, reflex and autonomic dysfunctions. Is adhesive arachnoiditis hereditary? Generally, adhesive arachnoiditis is not considered to be a hereditary disorder. However, it may be more likely to occur in people with a family history of similar disorders such as spondylolisthesis or joint hypermobility syndrome. It is also possible that genetic factors can play a role in the development of adhesive arachnoiditis, as some cases have been reported to be associated with connective tissue disorders.
Adhesive arachnoiditis is thought to be caused by a variety of factors, including physical trauma, repeated lumbar punctures, or surgery. It can also be caused by chemical irritation from certain medications, including corticosteroids, which are used to treat certain inflammatory conditions. The most common symptom of adhesive arachnoiditis is chronic pain, which can be felt anywhere from the lower back to the lower limbs. Other symptoms may include sensory deficits, weakness or paralysis of the limbs, bladder and bowel dysfunction, and cognitive impairment. Adhesive arachnoiditis is a serious condition that can have a significant impact on a person’s quality of life. Early diagnosis and treatment is important in order to manage symptoms and prevent further progression of the disease. Treatment generally includes medications, physical therapy, and lifestyle modifications.
What is the main cause of arachnoiditis?
The main cause of arachnoiditis is inflammation. It is believed that the inflammation is frequently caused by a chemical irritation or injury to the arachnoid membrane. Common causes of chemical irritation can include spinal surgery, injection of a substance, or exposure to a toxic substance. In some cases, the exact cause of arachnoiditis is unknown. This is known as idiopathic arachnoiditis.
In such cases, the inflammation may be related to a virus or an autoimmune disorder. In most cases, adhesive arachnoiditis only affects a small area of the spine. However, in some cases, it can spread to involve a larger area. If not managed properly, it can lead to permanent nerve damage and neurological deficits. Adhesive arachnoiditis is a serious condition that can cause chronic pain, neurological deficits and disability. Early diagnosis and prompt treatment can help reduce the risk of long-term complications.
How can you prevent arachnoiditis?
What is adhesive arachnoiditis? Adhesive arachnoiditis is a condition caused by inflammation of the arachnoid, which is a thin membrane that covers the spinal cord and nerve roots. This condition can cause severe pain, numbness, and weakness in the legs and arms. How can you prevent arachnoiditis? Fortunately, there are steps that you can take to reduce your risk of developing arachnoiditis. First, avoid activities that could lead to spinal trauma, such as contact sports, lifting heavy objects, and playing on uneven terrain. You should also take care to practice good posture, as this can reduce the amount of pressure that is placed on the spine.
Additionally, keep your spine healthy with a balanced diet and regular exercise. Furthermore, if you experience any back pain, it is important to seek medical attention as soon as possible to prevent further complications. Finally, it is important to be aware of any potential triggers that could cause an attack of arachnoiditis, such as certain medications, exposure to toxic agents, and even certain vaccinations. By taking steps to prevent these triggers, you can reduce your risk of developing arachnoiditis.
Does adhesive arachnoiditis go away?
What is adhesive arachnoiditis? It is a neurological disorder caused by inflammation of the arachnoid membrane, which is a membrane that covers the brain and spinal cord. It is most commonly caused by an infection in the central nervous system, or by a direct injury to the spine. The most common symptom of adhesive arachnoiditis is severe and chronic pain, usually in the neck and back. Other symptoms may include muscle weakness, numbness, tingling, and bladder and bowel problems. Adhesive arachnoiditis is a long-term chronic condition, and there is no cure.
Treatment usually consists of managing the pain with medications, physical therapy, and surgery. So, does adhesive arachnoiditis go away? Unfortunately, no. Because it is a chronic condition, it will not go away on its own. However, the symptoms can be managed with treatment, so the condition can be managed and the person’s quality of life improved.
Does arachnoiditis appear suddenly?
Symptoms of arachnoiditis can vary from mild to severe and can include pain, numbness, tingling, muscle weakness, and bladder, bowel and sexual dysfunction. This condition is also associated with psychological issues, such as depression, anxiety, and impaired cognitive functioning. Arachnoiditis can be caused by a variety of factors, including surgical procedures, infections, trauma, and the use of certain medications. In some cases, it may develop without any obvious cause. The diagnosis of arachnoiditis is based on a combination of the patient’s medical history, a physical examination, and imaging tests such as a CT scan or MRI.
Treatment usually involves medication and physical therapy, although surgery may be necessary in some cases. In summary, adhesive arachnoiditis is a long-term neurological disorder that can appear suddenly, and is associated with a range of symptoms. It can be caused by a variety of factors, and diagnosis and treatment usually involve a combination of medication and physical therapy.
What are the symptoms of adhesive arachnoiditis
The most common symptom of adhesive arachnoiditis is chronic pain that can range from mild to severe. Other symptoms may include burning sensations, tingling or numbness, muscle weakness and difficulty with coordination. In some cases, people may also experience bladder or bowel issues, sexual dysfunction and/or depression. Adhesive arachnoiditis can also cause difficulty in movement. This can be seen in the form of muscle spasms, paralysis, or an inability to move certain muscles.
In severe cases, people with adhesive arachnoiditis may experience paralysis of the lower body. Diagnosis of adhesive arachnoiditis is often difficult as the symptoms can be similar to other conditions. Imaging tests, such as an MRI or CT scan, can be used to diagnose the condition. A doctor may also perform a spinal tap or other tests to confirm the diagnosis. Treatment for adhesive arachnoiditis usually involves a combination of medications, physical therapy, surgery and lifestyle changes. Medications can include pain relievers, anti-inflammatories, muscle relaxants and antidepressants. Surgery may be necessary to remove scar tissue and/or reduce pressure on the spinal cord. Physical therapy and lifestyle changes can help reduce pain and improve mobility.
What is the difference between arachnoiditis and adhesive arachnoiditis?
Adhesive arachnoiditis is a specific type of this disorder where inflammation and scarring cause the arachnoid to stick to the dura mater, another membrane surrounding the spinal cord. The symptoms of arachnoiditis can include pain, numbness, tingling, and paralysis in the affected areas. Adhesive arachnoiditis generally causes more severe symptoms due to the additional damage caused by the adhesion of the arachnoid to the dura mater. Arachnoiditis can be caused by a number of different factors, including trauma, infection, or exposure to certain chemicals or drugs. Adhesive arachnoiditis is most commonly caused by repeated episodes of inflammation or irritation, such as repeated lumbar punctures, or spinal surgery.
The treatment of adhesive arachnoiditis is similar to that of arachnoiditis, but can also involve more invasive treatments such as spinal cord stimulation or epidural injections. In some cases, surgery may be needed to remove adhesions or scar tissue. To summarize, the main difference between arachnoiditis and adhesive arachnoiditis is that adhesive arachnoiditis involves an additional factor of the arachnoid adhering to the dura mater, which causes more severe symptoms and can require more invasive treatments.
What causes arachnoiditis to flare up?
As a result of this inflammation, the arachnoid can become overly adhesive, leading to a condition known as adhesive arachnoiditis. The exact cause of arachnoiditis flare-ups is not known, but experts believe that it is likely due to a combination of factors such as exposure to certain chemicals, trauma to the spine, or surgical interventions. It is also thought that underlying genetic factors may play a role in triggering the condition. Research has shown that the most common symptom of adhesive arachnoiditis is chronic pain, which can range from mild to severe. Other common symptoms include muscle weakness and spasms, numbness and tingling, abnormal sensations of skin crawling, and bladder and bowel problems.
Flare-ups of arachnoiditis can be triggered by stressful events, exposure to cold or hot temperatures, heavy physical activity, or even emotional stress. It is believed that these triggers stimulate the nerves and cause them to become overly sensitive, which can lead to an increase in pain and other symptoms. Unfortunately, adhesive arachnoiditis is a very complex disorder, and there is no known cure. However, there are treatments available to help manage and reduce the pain, including medications, physical therapy, and lifestyle changes. With the right combination of treatments, people can often manage their symptoms and live a productive life.
What are the most common symptoms of arachnoiditis?
The most common symptoms of arachnoiditis are: shooting or burning pains in the lower back, legs, and feet; numbness or tingling in the legs and feet; muscle weakness or spasms; difficulty walking; and bladder and bowel problems. These symptoms often worsen over time, leading to increasing pain and disability. Other symptoms include: depression; chronic fatigue; cognitive difficulties; inability to concentrate; difficulty sleeping; and an overall decline in the quality of life. These symptoms can be debilitating and can make it difficult to participate in daily activities. Adhesive arachnoiditis can be caused by injury or infection, as well as by surgery or other medical procedures, radiation therapy, or the use of certain medications.
Diagnostic tests such as an MRI or CT scan can be used to confirm the diagnosis. Treatments for arachnoiditis include pain medications, physical therapy, and nerve blocks. Surgery may be recommended in certain cases. In addition, a range of lifestyle changes can help to reduce pain and improve mobility.
How to treat adhesive arachnoiditis?
Symptoms of adhesive arachnoiditis can include pain in the lower back and legs, difficulty walking, loss of sensation and bladder control, and paralysis of the lower body. Treating adhesive arachnoiditis is a challenge because there is no known cure. The goal of treatment is to reduce inflammation, control pain, and help the patient maintain a good quality of life. Treatment options include physical therapy, medications, nerve blocks, and surgery. Physical therapy is often used to help strengthen muscles, reduce pain, and improve mobility.
Medications can also be used to reduce inflammation and pain. Nerve blocks can be used to relieve pain by blocking the nerve signals that cause the discomfort. Surgery may be recommended if other treatments are not effective. In addition to these treatments, lifestyle changes may also be beneficial. These may include exercise and stretching to improve muscle strength and flexibility, quitting smoking to reduce inflammation and improve circulation, and eating a healthy diet to reduce pain and inflammation. Adhesive arachnoiditis can be a difficult condition, but with the right treatment, patients can manage their symptoms and improve their quality of life.
What causes severe pain in the arachnoid bone?
Severe pain can be a symptom of adhesive arachnoiditis, which is caused by the inflammation of the arachnoid bone. This bone is a thin layer that encases the spinal cord, and it can be damaged due to a previous injury, infection, or inflammation. This can lead to inflammation of the arachnoid bone, which can cause a severe pain that is often described as unbearable. The pain can be either localized or radiate outward, and depending on the severity of the inflammation, it can be accompanied by other symptoms such as numbness and tingling. If the inflammation is severe, it can even cause paralysis or other neurological deficits.
Adhesive arachnoiditis can be treated with anti-inflammatory medications, analgesics, and physical therapy. Surgery is sometimes recommended if the pain is severe and not responding to other treatments. In conclusion, severe pain caused by adhesive arachnoiditis is often due to inflammation of the arachnoid bone, which can cause damage to the protective layer surrounding the spinal cord. Treatment includes medications, physical therapy, and surgery if necessary.
How does NINDS address arachnoiditis?
The National Institute of Neurological Disorders and Stroke (NINDS) is the main research agency of the National Institutes of Health (NIH) dedicated to researching and finding treatments for neurological disorders. NINDS is working to better understand the causes of adhesive arachnoiditis, as well as to develop treatments and improved care for those affected. NINDS is supporting research into the cause and progression of arachnoiditis, as well as seeking to improve treatment options. This includes research into drugs that may reduce inflammation, as well as strategies to reduce the pain associated with the disorder. NINDS is also supporting research into ways to diagnose arachnoiditis more quickly and accurately.
This includes testing new imaging techniques and clinical tests to enable earlier detection and more effective treatment. NINDS is committed to finding effective treatments and improved care for those affected by adhesive arachnoiditis. With continued research and clinical trials, NINDS is hopeful that better treatments and improved outcomes for people living with this condition can be achieved.